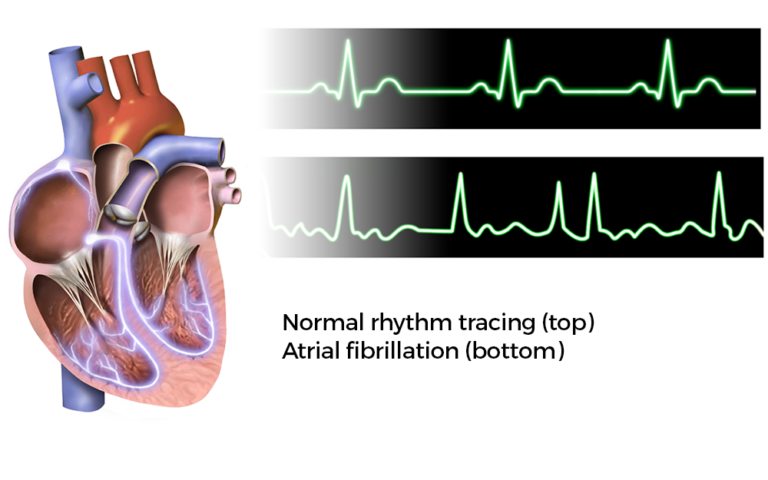
Atrial fibrillation (AFib or AF) is the most common type of arrhythmia. An arrhythmia is a problem with the rate or rhythm of your heartbeat. During an arrhythmia, your heart can beat too fast, too slow, or with an irregular rhythm.
AFib occurs if rapid, disorganized electrical signals cause the heart’s two upper chambers — called the atria — to fibrillate. The term “fibrillate” means to contract very fast and irregularly.
In AFib, blood pools in the atria. It isn’t pumped completely into the heart’s two lower chambers, called the ventricles. As a result, the heart’s upper and lower chambers don’t work together as they should.
People who have AFib may not feel symptoms. However, even if you don’t know you have AFib, it can increase your risk of stroke. In some people, AFib can cause chest pain or heart failure, especially if your heart rhythm is very rapid. AFib may happen rarely or every now and then, or it may become a chronic or long-term heart problem that lasts for years.
CardioVisual app for iPhone or CardioVisual for Android.[/action]
What Causes Atrial Fibrillation?
Atrial fibrillation (AF) occurs if the heart’s electrical signals don’t travel through the heart in a normal way. Instead, they become very rapid and disorganized. Damage to the heart’s electrical system causes AF. The damage most often is the result of other conditions that affect the health of the heart, such as high blood pressure and coronary heart disease. The risk of AF increases as you age. Inflammation is also thought to play a role in causing AF. Sometimes, the cause of AF is unknown.
Major Risk Factors
The risk of AF increases as you age and it’s more common in people who have:
- High blood pressure
- Coronary artery disease (CAD)
- Heart failure
- Rheumatic heart disease
- Structural heart defects, such as mitral valve prolapse
- Pericarditis, a condition in which the membrane, or sac, around your heart is inflamed
- Congenital heart defects
- Sick sinus syndrome — a condition in which the heart’s electrical signals don’t fire properly and the heart rate slows down. Sometimes the heart will switch back and forth between a slow rate and a fast rate.
- AF also is more common in people who have heart attacks or who have just had surgery.
- Conditions such as hyperthyroidism (too much thyroid hormone), obesity, diabetes, lung disease and sleep apnea.
- Alcohol and caffeine or psychological stress may also trigger AF in some people.
- Genetic factors also may play a role in causing AF. However, their role isn’t fully known.
Signs and Symptoms of Atrial Fibrillation
- Palpitations (a feeling that your heart is skipping a beat, fluttering, or beating too hard or fast)
- Shortness of breath
- Weakness or problems exercising
- Chest pain
- Dizziness or fainting
- Fatigue (tiredness)
- Confusion
Atrial Fibrillation Complications
AFib has two major complications—stroke and heart failure.
Stroke: During AF, the heart’s upper chambers, the atria, don’t pump all of their blood to the ventricles. Some blood pools in the atria. When this happens, a blood clot (also called a thrombus) can form. If the clot breaks off and travels to the brain, it can cause a stroke. (A clot that forms in one part of the body and travels in the bloodstream to another part of the body is called an embolus). Blood-thinning medicines that reduce the risk of stroke are an important part of treatment for people who have AF.
Heart failure Heart failure occurs if the heart can’t pump enough blood to meet the body’s needs. AF can lead to heart failure because the ventricles are beating very fast and can’t completely fill with blood. Thus, they may not be able to pump enough blood to the lungs and body. Fatigue and shortness of breath are common symptoms of heart failure, which are caused by a buildup of fluid in the lungs. Fluid can also build up in the feet, ankles, and legs, causing weight gain.
How Is Atrial Fibrillation Treated?
Treatment for atrial fibrillation (AF) depends on how often you have symptoms, how severe they are, and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
Specific Types of Treatment
Blood clot prevention: Preventing blood clots from forming is probably the most important part of treating AF.
Rate control: Rate control is the recommended treatment for most patients who have AF, even though an abnormal heart rhythm continues and the heart doesn’t work as well as it should. Most people feel better and can function well if their heart rates are well-controlled.
Rhythm control: Restoring and maintaining a normal heart rhythm is a treatment approach recommended for people who aren’t doing well with rate control treatment.
Procedures: Doctors use several procedures to restore a normal heart rhythm. For example, they may use electrical cardioversion to treat a fast or irregular heartbeat. Before doing electrical cardioversion, your doctor may recommend transesophageal echocardiography (TEE).
Catheter ablation may be used to restore a normal heart rhythm if medicines or electrical cardioversion don’t work.
New procedures (called left atrial appendage closure) to prevent clot from forming inside the heart in those patients who cannot take blood thinners are also being performed in some patients.
Approaches To Treating Underlying Causes and Reducing Risk Factors
Your doctor may recommend treatments for an underlying cause of AF or to reduce AF risk factors. Limiting or avoiding alcohol, caffeine, or other stimulants that may increase your heart rate also can help reduce your risk for AF.